CAIRS: A new take on corneal inserts

Pregnancy & Keratoconus
March 18, 2022
Eye Banks in the Time of COVID
March 30, 2022Originally published in NKCF Update (February 2022).
Intacs (intrastromal ring segments) are used by surgeons to change the shape of corneas. While these thin, plastic inserts do not stop KC progression, they can help to improve vision by decreasing the steepness of keratoconic eyes.
A few years ago, Dr. Soosan Jacob MD, a cornea surgeon in India described CAIRS (Corneal Allogenic Intrastromal Ring Segment), an arc-shaped insert made from collagen. Performed by a handful of ophthalmologists worldwide, CAIRS surgery using donor cornea tissue may eventually replace plastic inserts.
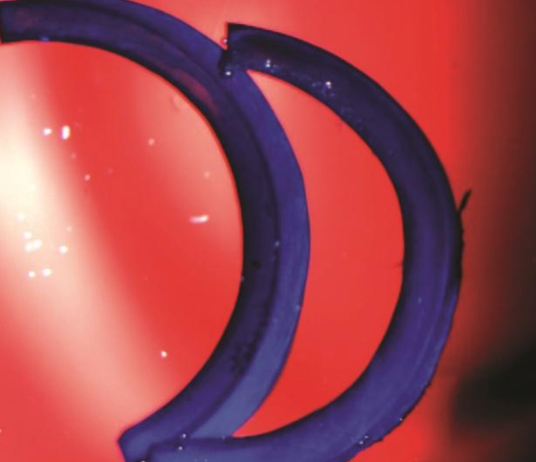
 Dr. Jack Parker MD, of Parker Cornea in Birmingham, AL is the most experienced CAIRS surgeon in the U.S. He has introduced a few advancements to streamline the surgical process. Dr. Parker works with the Alabama Eye Bank to prepare tissue for surgery. Technicians take donor corneas and remove the top (epithelium) and bottom (endothelium) layers. A trephine is used to create a circle of tissue and the circle is cut into two segments. The tissue is stained with a temporary blue dye to make it easier for the surgeon to see if the CAIRS is correctly placed.
Dr. Jack Parker MD, of Parker Cornea in Birmingham, AL is the most experienced CAIRS surgeon in the U.S. He has introduced a few advancements to streamline the surgical process. Dr. Parker works with the Alabama Eye Bank to prepare tissue for surgery. Technicians take donor corneas and remove the top (epithelium) and bottom (endothelium) layers. A trephine is used to create a circle of tissue and the circle is cut into two segments. The tissue is stained with a temporary blue dye to make it easier for the surgeon to see if the CAIRS is correctly placed.
Using a laser or a special blade, the surgeon creates a channel or tunnel in the cornea stroma and slips in the CAIRS. Dr. Parker has been performing this procedure on patients with keratoconus for three years with success. “The pool of patients who benefit from CAIRS compared to those who are appropriate for Intacs surgery is much greater. Some patients are not good candidates for Intacs because their corneas are too think or too steep for the plastic. CAIRS surgery works for these patients because the insert is made of cornea tissue,” according to Parker. The time in the operating room is somewhat longer than Intacs surgery, but he has been very happy with the results. “Since the CAIRS are not as rigid as the plastic Intacs, threading the tissue into the channel takes some effort; it can be like pushing a noodle. But I have not seen the scarring, glare or the discomfort that occasionally results after Intacs.”
Parker believes the donor tissue is more easily accepted by the recipient’s eye. The inserted tissue does not dissolve but remains stable within the stroma. The change in shape and stiffening to the recipient’s cornea is more natural. And since only a segment of donated cornea is used, it is possible that a single cornea donor can provide tissue used to improve the vision of several patients.