Corneal Transplant Surgery
Corneal transplant surgery has been successfully performed for more than 100 years. The surgery is recommended for the most advanced cases of keratoconus,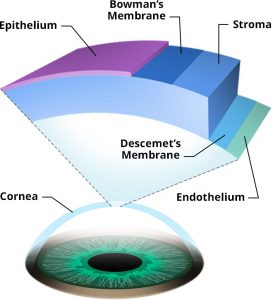 where the disease has progressed to the point where corneal thinning or steepening is extreme and scarring or a ‘cone’ or protrusion has formed. For these patients, it will be difficult to achieve good vision, and contact lens wear is often painful. Replacing the damaged cornea with a donor graft is a consideration for about 10-15% of individuals with keratoconus. It was generally a very successful surgery: more than 90% of transplant patients achieve a clear cornea and significant improvement in vision and eye comfort.
where the disease has progressed to the point where corneal thinning or steepening is extreme and scarring or a ‘cone’ or protrusion has formed. For these patients, it will be difficult to achieve good vision, and contact lens wear is often painful. Replacing the damaged cornea with a donor graft is a consideration for about 10-15% of individuals with keratoconus. It was generally a very successful surgery: more than 90% of transplant patients achieve a clear cornea and significant improvement in vision and eye comfort.
Until recently, keratoconus was the primary indication for corneal transplant surgery in the US. The Eye Bank Association of America reported there were 7,000 transplants performed for keratoconus and ectasia in 2011; that number fell to a little over 2,700 by 2019. KC is now the 6th most common indication for transplant surgery. At least two factors may have an impact. The use of custom contact lenses including scleral lenses has become more prevalent. Patients who were unable to tolerate contact lenses are now achieving good vision correction and comfort with lenses that accommodate damaged corneas. And, since corneal crosslinking was introduced, far fewer cases of keratoconus advance to the stage where a corneal transplant is the only alternative. Today, only patients with the most severe cases of keratoconus should expect to need a corneal transplant.
Despite the decline in numbers, there are still individuals with keratoconus who benefit from a corneal transplant. Patients should discuss all possible options with their eyecare professional. Your doctor will explain the type of surgery you will have and what to expect. Corneal transplant surgery for keratoconus is elective (non-emergency) surgery, so a delay while you consider your options should not affect the outcome. This is a time to ask questions and consider getting a second medical opinion so that you have the information needed to make a decision that fits your situation.
Where do the donor corneas come from?
Cornea tissue is retrieved from a recently deceased organ donor. Retrieval occurs within a few hours of death. The cornea (not the entire eye) is removed by a technician and brought to an ‘eye bank’ for processing. Cornea cells are assessed under a microscope for overall health and quality. Testing is also performed to assure the cornea is disease-free and safe for transplant. The tissue is then sterilized and prepared for shipment to the eye surgeon. There is no donor match needed for corneas. Transplant surgery normally occurs within two or three days of the donor’s death.
What happens in cornea transplant surgery?
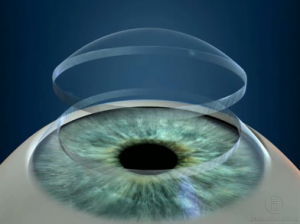
 The cornea is the transparent, dome-shaped outer cover to the eye. It is thinner than a credit card and consists of 5 cell layers, each with a different purpose. A cornea transplant replaces the damaged cornea with healthy donor tissue. The surgery takes about two hours and is usually performed in an outpatient or ambulatory surgery center.
The cornea is the transparent, dome-shaped outer cover to the eye. It is thinner than a credit card and consists of 5 cell layers, each with a different purpose. A cornea transplant replaces the damaged cornea with healthy donor tissue. The surgery takes about two hours and is usually performed in an outpatient or ambulatory surgery center.
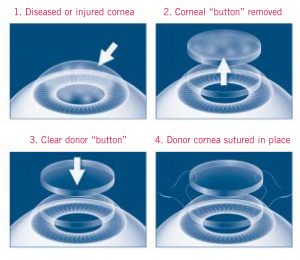
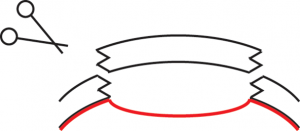
The eye surgeon uses a trephine, a small circular blade to remove a round portion of the damaged cornea and replaces it with a similar graft cut to match. Many eye surgeons and eye banks coordinate efforts and use a special laser to cut precise patterns in the tissue so the graft fits like a jigsaw puzzle piece. Using a microscope, the surgeon sutures the replacement cornea in place. An eye patch or eye
shield is put over the eye and the patient discharged with a follow-up appointment for the next day. There are generally two types of transplant surgery considered in cases of advanced keratoconus.
In PK, the entire full thickness (5 layers) of the cornea is replaced by donor tissue. PK is preferred when keratoconus has scarred or damaged the back layers of the cornea. The wound heals gradually, and your doctor may choose to remove some or all the sutures over several months. Sometimes the stitches are left in place permanently, depending on how quickly the graft heals, the type of stitches used, and the health and vision of the eye. This procedure is easier for the surgeon to perform, and is the most common type of corneal transplant for treatment of advanced KC.
Often only the top portions of the cornea are damaged, while the bottom layer (endothelium) is still healthy. In DALK, the surgeon delicately separates the donor tissue during surgery and the only top portions of the cornea are replaced. This surgery is technically challenging and should be performed by eye surgeons who are experienced in the procedure. Because the bottom 5% of the patient’s cornea remains in place, successful DALK surgery results in shorter healing time and less chance of a graft rejection.
![]()
![]()

What happens after the surgery?
Corneal transplant surgery is highly successful, but because the cornea has no blood supply, the transplant heals relatively slowly. It may be months to a year before stable vision is achieved.
For the first few days, expect your eye to be red, irritated, and sensitive to light. It may feel gritty and your vision may seem worse. You will be given eyedrops or ointments to help your eye heal. Antibiotics will prevent infection and steroids will reduce swelling, inflammation, and prevent rejection.
Your surgeon will recommend that you wear eyeglasses or other protective eyewear for a period after surgery and avoid activities that could result in trauma or a direct blow to the eye. You may be directed to avoid heavy pushing and pulling during the first few weeks after surgery. Avoiding eye rubbing is essential a successful outcome.
Will I still need glasses after the surgery?
Many patients are under the misperception that replacing their damaged cornea with healthy donor tissue will mean they will have perfect uncorrected vision. While vision will likely improve, most patients still wear eyeglasses or contact lenses for vision correction. Although vision may not be perfect after surgery, it is nearly always an improvement over the pre-operative vision.
Is my keratoconus cured after transplant surgery?
In a very small number of cases, keratoconus may recur. Doctors have reported evidence of graft protrusion many years after the original transplant surgery. The reemergence of KC is not necessarily the result of incomplete removal of the cone during the original surgery. For some patients with aggressive KC, disease progression does not necessarily stop when a corneal transplant is performed. In these rare cases, keratoconus cells are thought to slowly migrate from the host (patient) to the donor
tissue. Corneal crosslinking may be recommended for these patients. Another factor that has resulted in recurrence of KC is continued eye rubbing.
What are the risks of corneal transplant surgery?
As with all medical procedures, there are risks that your doctor will describe. The most significant associated with corneal transplant is graft rejection. The risk is small and may occur years after surgery. Graft rejection occurs when a body attacks the transplanted tissue. The symptoms are best remembered by the letters RSVP.
Increased REDNESS
Extreme SENSITIVITY to light
Decreased VISION
Increased eye PAIN
At the first sign of rejection, contact your eye surgeon. Medicated eye drops, started soon enough, are usually successful in reversing rejection.
Another serious risk is graft failure when the transplanted tissue becomes cloudy. Graft failure does not mean that the cornea will fall out, but there can be serious loss of vision. Repeat corneal transplants are normally possible, but each successive transplant surgery increases the likelihood of a less than satisfactory outcome. For these risks and others, it is important to continually monitor the health of the graft over your lifetime.
How long before I need to replace the transplanted cornea?
With proper care and attention to any sign of rejection or failure, a cornea graft can last a lifetime. The length of time a corneal graft remains healthy is based on several factors. Corneal transplants for progressive keratoconus seem to be among the most successful corneal transplants performed. It is not unusual to find patients with keratoconus who have had their graft in place for over 30 years.