CXL Redo: Retreatment After Crosslinking

A Caution About Eyelash Extensions
November 19, 2021
Cataract Surgery & Keratoconus
December 17, 2021Originally published in NKCF Update (May 2020)
Two recent articles published in the journal Cornea called attention to an infrequent adverse event – progression of keratoconus (KC) after corneal crosslinking (CXL). No medical procedure can guarantee a desired outcome, but CXL offers a remarkable chance of success. CXL is safe, effective, and complication-free in a majority of cases.
 Researchers from the Netherlands examined the medical records of 460 patients with progressive KC between 2010 and 2016. These patients were treated using different CXL modalities including the Dresden protocol (the epithelium-off method), as well as variations of epithelium-on, and treatment combinations where the intensity of ultraviolet light or the riboflavin (vitamin B) formulation was altered. The authors followed these patients after treatment and considered an increase in the maximum keratometry (Kmax) of ≥1.00 diopter a less than successful outcome.
Researchers from the Netherlands examined the medical records of 460 patients with progressive KC between 2010 and 2016. These patients were treated using different CXL modalities including the Dresden protocol (the epithelium-off method), as well as variations of epithelium-on, and treatment combinations where the intensity of ultraviolet light or the riboflavin (vitamin B) formulation was altered. The authors followed these patients after treatment and considered an increase in the maximum keratometry (Kmax) of ≥1.00 diopter a less than successful outcome.
Patients who showed signs of progression were advised to have a repeat CXL. Retreatment is simply redoing the CXL treatment. Thirteen patients out of 460 required retreatment. Different treatment protocols yielded different rates of success, yet no protocol was superior to the standard Dresden epi-off procedure.
Dr. Vasilios Diakonis, MD, PhD, a cornea specialist at the Eye Institute of West Florida was not surprised by these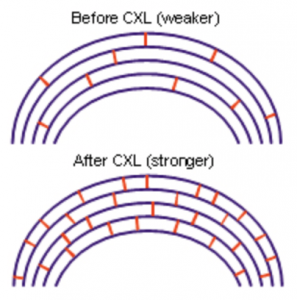 results, noting the Dresden protocol has demonstrated a 90+% success rate for halting progression of KC. He observed, “Only a small population of patients may require a retreatment which will most likely stop progression.”
results, noting the Dresden protocol has demonstrated a 90+% success rate for halting progression of KC. He observed, “Only a small population of patients may require a retreatment which will most likely stop progression.”
In a second article, doctors in a Turkish university looked at the results of repeated corneal crosslinking for progressive KC. They reported that of 800 patients treated with CXL, 12 eyes (10 patients from age 14 to 34) required retreatment because of Kmax progression of ≥1.00 diopter. The steepening took place between one and four years after the initial CXL. After the 12 retreatments, 8 showed improvement, 2 were stabilized, and 2 eyes continued to show progression of disease.
In addition to individuals who continue to rub their eyes, Dr. Diakonis added that younger patients are the ones most likely to need retreatment. He said, “The corneal stroma has a tissue turnover of 7 years, crosslinking thereby stiffens corneal tissue for a 7- year period. The older a patient gets, the more stiff the cornea gets due to aging. Younger patients are more prone to demonstrate progression of keratoconus.”
Dr. Christopher Hood, MD, associate professor of ophthalmology at the University of Michigan’s Kellogg Eye Center performs CXL on a diverse patient population. He agrees with that observation. “Of the five retreatments I have performed, all of these patients had their initial CXL when they were under the age of 21.” He also reports that the patients who need retreatment are often those who did not initially have the FDA-approved protocol. “All of the patients who were referred to Kellogg Eye Center for retreatment had epithelium-on procedures elsewhere; some in combination with PRK (photorefractive keratectomy, a vision correction surgery).” Dr. Hood performs the Dresden protocol and all the patients he retreated have shown no new signs of disease progression. 
CXL is a proven method to treat progression of keratoconus. Depending on the techniques employed, the success rate can exceed 90%, and if retreatment is required, it can be performed without difficulty and little risk.
It is important to remember that CXL does not guarantee that progression will not occur months and even years after treatment. If you have undergone CXL, make sure you continue to follow-up with your eye doctor who will monitor your eye for changes and advise you if retreatment is recommended.
References:
Godefrooij DA, Roohe SL, Soeters N, Wisse RPL, The Independent Effect of Various Cross-Linking Treatment Modalities on Treatment Effectiveness in Keratoconus, Cornea, 39:63-70, 2020
Turhan SA, Aydin FO, Toker E, Clinical Results of Repeated Corneal Collagen Cross-linking in Progressive Keratoconus, Cornea, 39:84-87, 2020
 Dr. Vasilios Diakonis, MD, PhD was born in New York and received his medical degree and doctorate in refractive surgery in Greece. He completed a research and clinical fellowship in cornea disease at the Bascom Palmer Eye Institute in Miami and now treats patients at the Eye Institute of West Florida with offices in Tampa, Largo, and St. Petersburg.
Dr. Vasilios Diakonis, MD, PhD was born in New York and received his medical degree and doctorate in refractive surgery in Greece. He completed a research and clinical fellowship in cornea disease at the Bascom Palmer Eye Institute in Miami and now treats patients at the Eye Institute of West Florida with offices in Tampa, Largo, and St. Petersburg.
 Dr. Christopher Hood, MD is Clinical Associate Professor of Ophthalmology at the University of Michigan. He is Medical Director of the Cornea and Refractive Surgery Clinic at the Kellogg Eye Center in Ann Arbor. Dr. Hood is a graduate of the University of Michigan Medical School and completed his residency at the Cleveland Clinic and cornea fellowship at University of Michigan.
Dr. Christopher Hood, MD is Clinical Associate Professor of Ophthalmology at the University of Michigan. He is Medical Director of the Cornea and Refractive Surgery Clinic at the Kellogg Eye Center in Ann Arbor. Dr. Hood is a graduate of the University of Michigan Medical School and completed his residency at the Cleveland Clinic and cornea fellowship at University of Michigan.



