Cataract Surgery & Keratoconus

CXL Redo: Retreatment After Crosslinking
December 10, 2021
New Scleral Lens Product
January 6, 2022Originally published in NKCF Update (May 2020).
For most people, cataracts are a natural part of the aging process. More than 90% of those over the age of 65 show some evidence of a cataract. As cataracts develop, the natural lens, which sits behind the cornea and iris, becomes cloudy and vision can become hazy, colors become muted, and night vision becomes a challenge.
During surgery, the cloudy natural lens is replaced with a clear, artificial lens. This outpatient procedure is generally safe and effective. In the US, close to 4 million cataract procedures are performed each year, making it the most performed surgery. 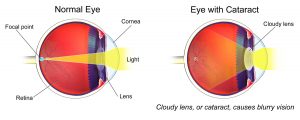
Individuals with keratoconus (KC) have no different risk of developing cataracts than the general population and should expect to develop cataracts as they age. It seems like having the cataract removed and the lens replaced would be an easy decision for most seniors, but for individuals with KC, the idea of any surgery to the eye can be troubling.
“That should not be the case,” says Dr. Sam Garg, MD, a cornea specialist at the UC-Irvine Gavin Herbert Eye Institute.
In cataract surgery, the surgeon makes a micro incision in the cornea – less than 1/8 of an inch. Through this tiny opening, the surgeon will both remove the cloudy lens and insert the new artificial lens. While most cataract surgeries do not even require a stitch to close the incision, Dr. Garg notes some surgeons may put a single stitch across the cornea incision to assure prompt wound healing when performing cataract surgery on their patients with KC.
“Because the keratoconus eye can act a little differently than a normal eye, we want to make sure the wound seals appropriately and there are no complications,” says Dr. Garg.
He notes the most important element in ensuring successful cataract surgery for individuals with KC is the precise selection of a replacement lens.
There are two important elements to consider in choosing the proper artificial lens. Well before surgery, the eye doctor will discuss vision priorities. For many, it is important to restore distance vision and the patient is content to use reading glasses for close work. Other patients prefer a replacement lens that will offer improved vision at multiple distances.
After this discussion, the doctor takes measurements of the eye, including the shape of the cornea and length of the eye. Using well-established algorithms, the surgeon selects an artificial lens that best meets the patient’s needs. Dr. Garg adds that the choice of the lens should be personalized, based on needs, desires, and suitability.
For individuals with moderate to severe KC who achieve good vision with contact lenses, the goal may be to return to their contact lenses. For those with mild cases of KC, some improvement in vision may be accomplished so that the patient can function with eyeglasses postoperatively. Replacement lenses that offer correction of astigmatism may not be appropriate if the cornea is highly irregular, which is the case for those with severe KC (and even some cases of mild/moderate KC).
Selecting the right replacement lens, based on the pre-operative measurements takes expertise. The normal algorithms that surgeons employ do not translate easily to the irregular eye. Making the proper preoperative calculations is essential to finding the optimal replacement lens.
There are other special situations that may impact the individuals with KC. Patients who have undergone a corneal transplant can develop cataracts and undergo surgery successfully. Since any surgery results in endothelial cell loss, cataract surgeons are careful to test the health of the corneal graft before surgery. Likewise, patients who have had intrastromal rings (INTACS) placed can undergo cataract surgery. In some cases, these rings are removed prior to the cataract surgery; this becomes another factor your surgeon must consider in selecting the right replacement artificial lens.
Dr. Garg notes that doctors are still learning about cataract surgery in crosslinked eyes. “We have seen that eyes that have undergone crosslinking continue to flatten after the procedure. These changes in shape influence the selection of a replacement lens.” He noted that as our experience with crosslinking grows, our understanding of how this impacts choice of an optimal replacement lens will also increase.
have undergone crosslinking continue to flatten after the procedure. These changes in shape influence the selection of a replacement lens.” He noted that as our experience with crosslinking grows, our understanding of how this impacts choice of an optimal replacement lens will also increase.
Those living with keratoconus should expect to be develop cataracts as they age. They need not avoid surgery and live with diminished vision: 98% of patients report improved vision after surgery. Even those who have lived with KC for decades have an opportunity to experience improved eyesight. To get the best possible outcome, it is critical to select an eye surgeon who has experience working with KC patients and who understands the special considerations that apply.
 Dr. Sumit (Sam) Garg, MD is Associate Professor of Ophthalmology at UC Irvine. He is Medical Director and Vice Chair of Clinical Ophthalmology at the Gavin Herbert Eye Institute. Dr. Garg is an accomplished clinician, author and lecturer. As Chair of the ASCRS Young Eye Surgeons Committee, he teaches residents and fellows the latest techniques in cataract and refractive surgery. He serves as the Medical Director for National Keratoconus Foundation.
Dr. Sumit (Sam) Garg, MD is Associate Professor of Ophthalmology at UC Irvine. He is Medical Director and Vice Chair of Clinical Ophthalmology at the Gavin Herbert Eye Institute. Dr. Garg is an accomplished clinician, author and lecturer. As Chair of the ASCRS Young Eye Surgeons Committee, he teaches residents and fellows the latest techniques in cataract and refractive surgery. He serves as the Medical Director for National Keratoconus Foundation.


