Corneal Transplant Options: Penetrating Keratoplasty vs. Deep Anterior Lamellar Keratoplasty

Challenges Associated with Pediatric KC
January 22, 2024
Novel Nasal Spray Combats Dry Eye
January 30, 2024Corneal Transplant Options: Penetrating Keratoplasty vs. Deep Anterior Lamellar Keratoplasty
Originally published in NKCF Update (November 2023).
Surgeons at Shahid Beheshti University in Tehran compared results from 411 keratoconus patients who underwent corneal transplants between 1994 and 2020. The procedures were performed by a single, experienced cornea surgeon. All patients reported contact lens intolerance, had a best corrected visual acuity worse than 20/40, and severe cornea curvature with keratometry readings ≥ 60 diopters before surgery.
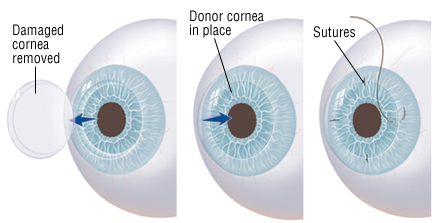
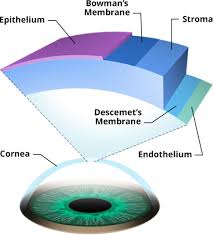
The paper, published in the April 2023 issue of the American Journal of Ophthalmology, compared two transplant techniques: penetrating keratoplasty (PK), a complete replacement of the cornea with donor tissue, and deep anterior lamellar keratoplasty (DALK) where only the top layers of the patient’s cornea are replaced with donor tissue.
 The paper compared outcomes of 218 eyes that underwent PK and 193 that received DALK. Both techniques resulted in significant vision improvement after surgery, slightly better for patients who underwent PK.
The paper compared outcomes of 218 eyes that underwent PK and 193 that received DALK. Both techniques resulted in significant vision improvement after surgery, slightly better for patients who underwent PK.
In about 1/3 of the cases reported in this series, the surgeon intended to perform DALK, but an intraoperative tear in Descemet’s membrane during the procedure resulted in ‘converting’ the DALK to a PK transplant. This rate is not unusual.
Both procedures require suturing around the donor cornea tissue. Suture-related complications like loosening or broken sutures occurred in both DALK and PK, more often in DALK eyes (72.0% vs. 48.6% in PK eyes).
At least one episode of graft rejection (pain, redness, light sensitivity) occurred in 33.5% of PK eyes and 19.7% of DALK eyes. The total number of rejection episodes over several years follow-up was 135 in the PK group and 74 in the DALK group. In most cases, steroid drops were given, and the rejection episodes were successfully managed. Graft failure resulting in a repeat transplant occurred in 4 PK eyes (1.8%) and 10 DALK eyes (5.2%).
One transplant in the DALK group and one in the PK group needed to be replaced because of recurrence of keratoconus. This serves as a reminder that, although rare, keratoconus can recur even after a cornea transplant.
This snapshot of one surgeon’s experience did not show obvious superiority of on technique over the other. DALK is a more complicated procedure for the surgeon to perform, but may result in fewer post-operative complications. PK is a well-established procedure and has been the standard of care for 70 years.
Advances in contact lens technology and cross linking have decreased the need for transplants except in the most advanced cases of keratoconus. Patients considering a corneal transplant for severe keratoconus should discuss possible complications and expected out comes with their surgeon preoperatively.
Reference: Penetrating Keratoplasty Versus Deep Anterior Lamellar Keratoplasty for Advanced Stage of Keratoconus, Feizi S, Javadi MA, Karimian F, et al, Amer J Ophthalmol, 248:107-115, 2023.